https://www.noonecoming.com/masks-respirators-and-covid19/
Masks, Respirators, and COVID19
Posted on April 14, 2020 by NOC Actual
Part 1
A few days ago, the CDC announced that all Americans should be wearing face coverings when out in public to prevent spread of COVID19. This announcement is widely recognized to mean that masks (rather than the vague “face covering”) are necessary to prevent, or slow, additional spread of the disease. This comes after weeks of the CDC and other authorities discouraging the public from obtaining and wearing masks, in a perhaps misguided effort to preserve resources for healthcare workers. These early comments emphasized the ineffectiveness of facemasks in preventing transmission of SARS-CoV-2 (the virus that causes COVID19), while at the same time championing the value of these items for healthcare workers. Many commentators and individuals at that time saw the dissonance in this paradoxical position, and many others have been quick to point out the airborne transmission potential of SARS-CoV-2.
We have known for weeks that SARS-CoV-2 could be transmitted on airborne particles, and not just through contact droplets. Keen observers will have made the connection for themselves that some type of mask is not paranoia but prudence. The announcement simply confirms what we have known for weeks, while simultaneously weakening faith in government management of the COVID19 pandemic.
The decision to discourage the American public from wearing respiratory protection seems to have been made in order to preserve capacity for healthcare workers. However, this failed to properly inform the public about the nature of their risk, and failed to account for the respiratory protection already in the hands of non-medical people or on store shelves and not in hospital stockrooms. Many businesses and workers outside of healthcare came into this pandemic with a supply of respiratory protection. Stocks of surgical masks, dust masks, N95 (and better) respirators on store shelves were bought up almost as fast as toilet paper, despite official efforts to discourage use. These items were never going to be available to hospital stocks in any circumstance, and discouraging individuals with access that didn’t impact hospital stocks was likely a mistake. The early and routine use of respiratory protection by the public could have had an impact on SARS-CoV-2 spread, and could have helped to flatten the curve even further. This would have in turn protected healthcare workers by reducing case load and exposure, or at least spreading it out enough for manufacturing to begin to catch up to the mask demand.
We can guess that it might have been so, at any rate. It is impossible to say for certain if this alternative would have created a better outcome, and now we must live with the decisions that were made. There are no truly good answers, and every decision comes with consequences.
Consider that the theme for this discussion of respiratory protection for SARS-CoV-2/COVID19. There are no good answers, and every decision comes with consequences. Welcome to 2020, a pandemic year in which we can look back at years of predictions that called for millions of face masks and respirators. Millions that were never stockpiled, never produced, and do not exist in our time of need. We have put ourselves in the position of having no good choices left.
What is Respiratory Protection?
In short, respiratory protection is any measure or device undertaken to prevent the inhalation (breathing in) of harmful materials. In particular, we are interested in face coverings which offer respiratory protection. Masks, respirators, N95s, N99, PM2.5, bandannas, face coverings, surgical masks, dust masks: What are all of these things, and what are the differences?
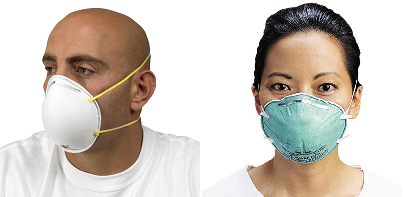
There are many types of masks designed to offer the wearer at least some protection from inhaled hazards in their environment. The most common are simple dust masks, which cover the nose and mouth with a thin layer of fabric or non-woven material to help filter dusts generated during cleaning, certain types of work, or manufacturing. The highest levels of protection are provided by masks called respirators, which come in several forms. Let’s run all of these down in brief.

The ideal among all of these types of masks, for protection against SARS-CoV-2, is an N95 (or better) rated filtering face-piece respirator, that properly fits the wearer. To work, the respirator must have a close, tight, fit to the face that does not allow any air to pass around the edges of the mask. All inhaled air must pass through the filter, for the filter to protect the wearer.
There are some design differences between these types of FFR’s that are worth noting. Many disposable N95 masks have a valve in the center of the mask, that allows exhaled air to directly exit the mask. This is a one-way vale that seals during inhalation. Strap design is also important, as dual-strap designs are the most effective at sealing against the wearers face. Single strap designs have more potential for improper fit.
In ideal circumstances, an N95 or better respirator should be properly fitted to the individual wearer in a process called fit testing. During the COVID19 pandemic, many users are not going to be able to receive a proper fit testing. Please see the section on respirator fitting and wear later in this article.
Masks, Respirators, and COVID19
Posted on April 14, 2020 by NOC Actual
Part 1
A few days ago, the CDC announced that all Americans should be wearing face coverings when out in public to prevent spread of COVID19. This announcement is widely recognized to mean that masks (rather than the vague “face covering”) are necessary to prevent, or slow, additional spread of the disease. This comes after weeks of the CDC and other authorities discouraging the public from obtaining and wearing masks, in a perhaps misguided effort to preserve resources for healthcare workers. These early comments emphasized the ineffectiveness of facemasks in preventing transmission of SARS-CoV-2 (the virus that causes COVID19), while at the same time championing the value of these items for healthcare workers. Many commentators and individuals at that time saw the dissonance in this paradoxical position, and many others have been quick to point out the airborne transmission potential of SARS-CoV-2.
We have known for weeks that SARS-CoV-2 could be transmitted on airborne particles, and not just through contact droplets. Keen observers will have made the connection for themselves that some type of mask is not paranoia but prudence. The announcement simply confirms what we have known for weeks, while simultaneously weakening faith in government management of the COVID19 pandemic.
The decision to discourage the American public from wearing respiratory protection seems to have been made in order to preserve capacity for healthcare workers. However, this failed to properly inform the public about the nature of their risk, and failed to account for the respiratory protection already in the hands of non-medical people or on store shelves and not in hospital stockrooms. Many businesses and workers outside of healthcare came into this pandemic with a supply of respiratory protection. Stocks of surgical masks, dust masks, N95 (and better) respirators on store shelves were bought up almost as fast as toilet paper, despite official efforts to discourage use. These items were never going to be available to hospital stocks in any circumstance, and discouraging individuals with access that didn’t impact hospital stocks was likely a mistake. The early and routine use of respiratory protection by the public could have had an impact on SARS-CoV-2 spread, and could have helped to flatten the curve even further. This would have in turn protected healthcare workers by reducing case load and exposure, or at least spreading it out enough for manufacturing to begin to catch up to the mask demand.
We can guess that it might have been so, at any rate. It is impossible to say for certain if this alternative would have created a better outcome, and now we must live with the decisions that were made. There are no truly good answers, and every decision comes with consequences.
Consider that the theme for this discussion of respiratory protection for SARS-CoV-2/COVID19. There are no good answers, and every decision comes with consequences. Welcome to 2020, a pandemic year in which we can look back at years of predictions that called for millions of face masks and respirators. Millions that were never stockpiled, never produced, and do not exist in our time of need. We have put ourselves in the position of having no good choices left.
What is Respiratory Protection?
In short, respiratory protection is any measure or device undertaken to prevent the inhalation (breathing in) of harmful materials. In particular, we are interested in face coverings which offer respiratory protection. Masks, respirators, N95s, N99, PM2.5, bandannas, face coverings, surgical masks, dust masks: What are all of these things, and what are the differences?
There are many types of masks designed to offer the wearer at least some protection from inhaled hazards in their environment. The most common are simple dust masks, which cover the nose and mouth with a thin layer of fabric or non-woven material to help filter dusts generated during cleaning, certain types of work, or manufacturing. The highest levels of protection are provided by masks called respirators, which come in several forms. Let’s run all of these down in brief.

- Dust Masks or Comfort Masks – Simple masks that provide the lowest levels of protection, filtering out only the largest of particles such as dust. Largely for increased wearer comfort in dusty environments, while affording no meaningful protection
- Surgical Masks and Procedure Masks – Loosely fitting, and allowing air to pass around the sides of the mask, surgical masks serve more as a physical barrier against large droplets, splashes, and sprays, than as any kind of filter. Surgical masks are designed to protect everyone but the wearer, by blocking exhaled particles from reaching other people are surfaces. Surgeons wear these not to protect themselves from pathogens you may carry, but to protect you from their snot dripping into your open body compartments during surgery. According to the CDC, in medical settings surgical masks are only used to prevent spread of aerosol particles from the mask’s wearer. They do not confer any protection to the wearer from particles from other people. To protect wearers from pathogens from others, N95 or better respirators must be used
- Air Purifying Respirators – Closely fitting masks which force inhaled air through a filter, to filter out the smallest of particles possible while still allowing breathing. This type of respirator is known as an Air Purifying Respirator, as it uses filtration to purify inhaled room air. The most common are N95 respirators, which filter out >95% of particles 0.3 microns or larger. Other grades, such as N99, filter out closer to >99%, while still others such as P95 filter out >95% while being oil-proof. (For a full list of respirator ratings, and more information on additional types, see Wikipedia). There are some types of air purifying respirator which fully enclose the wearer’s head in a full-face mask, providing eye protection as well. Some of these, Powered Air Purifying Respirators (PAPR) use forced air systems to draw air through filters into the enclosed head-piece
- There are additional categories of respirator called Air-Supplied Respirators, which amount to a self-contained-breathing-apparatus that provides purified air from a canister or supply, rather than drawing room air through a filter. For the purposes of this article, we are going to be discussing Air Purifying Respirators, and specifically filtering face-pieces
- There are other types of filtering face-pieces called pollution masks, which are relatively uncommon in the United States but very common in some other countries. Some of these are little more than a Comfort Mask, while others are often a washable close-fitting fabric mask, with disposable filter inserts. These masks are often marketed as PM2.5 masks, meaning they are designed to filter pollution particles 2.5 microns in size or smaller. However, the filters used for these masks are often N95 filters, designed to filter 0.3 micron particles. Not all pollution masks are N95-equal, however, and it’s important to know which masks of this type use filters, and which are true PM2.5, just fabric, or N95 or better. Many pollution masks also cannot pass fit testing, and provide ineffective filtration
- (Important note: Although many sources use the terms interchangeably, respirator and ventilator are not the same thing. A ventilator is a device used to push air into the lungs of a critically ill patient. A respirator is a filtering device that someone breathes through, to protect themselves from the finest of inhaled particles)
The ideal among all of these types of masks, for protection against SARS-CoV-2, is an N95 (or better) rated filtering face-piece respirator, that properly fits the wearer. To work, the respirator must have a close, tight, fit to the face that does not allow any air to pass around the edges of the mask. All inhaled air must pass through the filter, for the filter to protect the wearer.
There are some design differences between these types of FFR’s that are worth noting. Many disposable N95 masks have a valve in the center of the mask, that allows exhaled air to directly exit the mask. This is a one-way vale that seals during inhalation. Strap design is also important, as dual-strap designs are the most effective at sealing against the wearers face. Single strap designs have more potential for improper fit.
In ideal circumstances, an N95 or better respirator should be properly fitted to the individual wearer in a process called fit testing. During the COVID19 pandemic, many users are not going to be able to receive a proper fit testing. Please see the section on respirator fitting and wear later in this article.